9 Breathing Exercises to Try When You Feel Anxious
Breath is an essential aspect of living, and for the most part, we do it without any extra effort. As we inhale, blood cells become oxygenated and shed carbon dioxide. Incorrect breathing can disturb the exchange of oxygen and carbon dioxide and result in anxiety, panic attacks, tiredness and other physical and emotional health problems.
The next time you feel on edge, there are several anxiety breathing exercises that you could try. Find out how to utilize breathing techniques for reducing anxiety and stress. If you have a lung condition, such as COPD or asthma, or are in pain or having difficulty breathing, consult a health care professional before attempting any type of breathing exercise.
Anxiety disorders, which such as prove to be a pandemic by affecting an approximate 40 million adults in the US each year, are the most prevalent mental health disorder. The way that anxiety is experienced is different for everybody, but the physical symptoms often include an accelerated heart rate, higher blood pressure, and changes in how you’re breathing.
Here are nine doctor-approved breathing exercises you may want to incorporate into your exercise routine, backed by both clinical anecdote and research. These methods all address different components of the anxiety response, are easy to implement, and do not require special equipment or training.
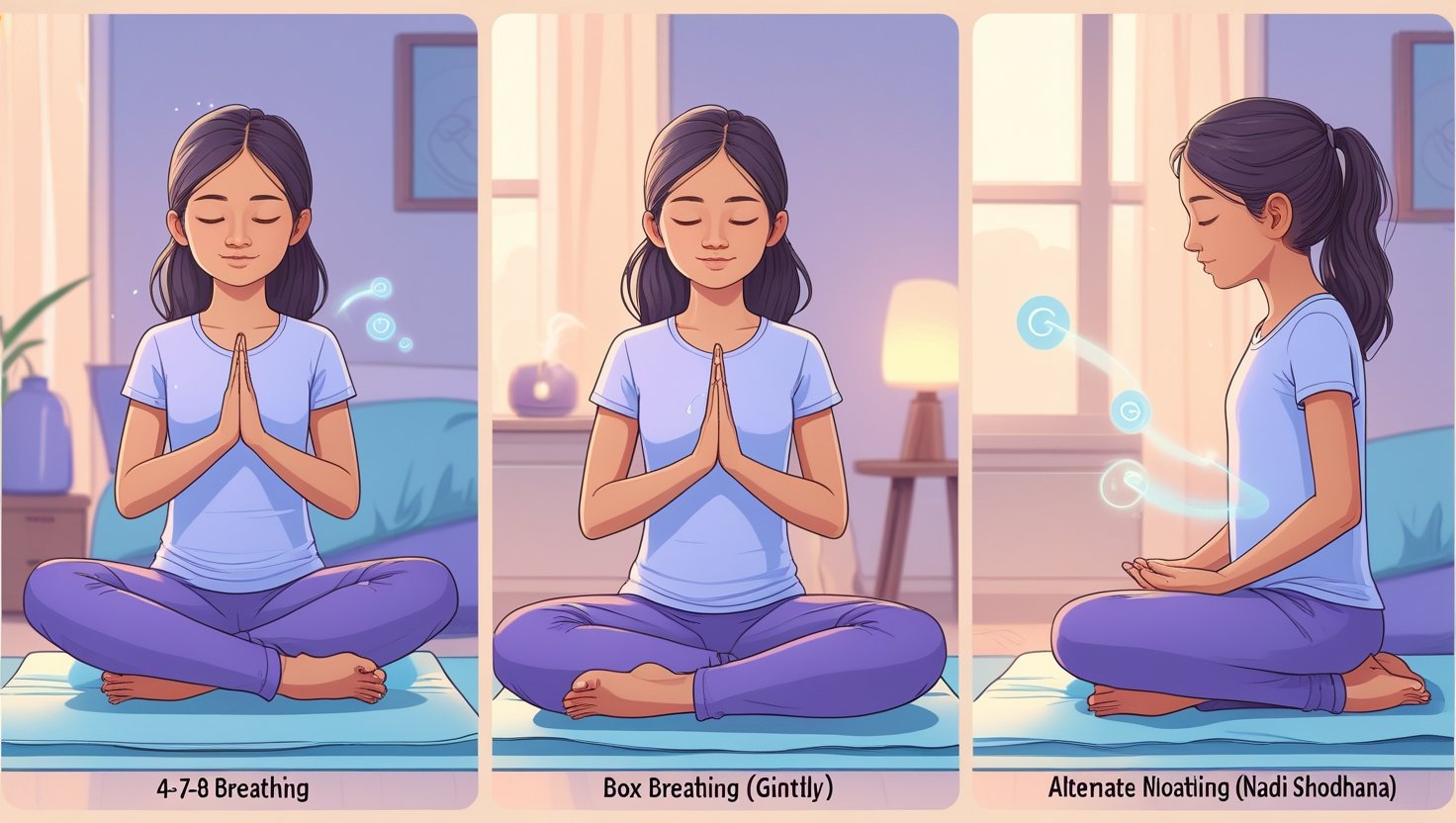
Alternate-Nostril Breathing

Anuloma-Viloma breathing (AVB), a form of alternate-nostril breathing (a pranayama technique, Nadi Shodhana), is one of several unilateral breathing techniques studied for effects on autonomic nervous system (ANS) balance. This is done by breathing in and out through one nostril at a time, manually occluding the opposite nostril.
Clinical Application:
Sit in any comfortable pose keeping the back straight.
- Close the right nostril by applying light pressure with the right thumb.
- Breathe in four counts through L nostril.
- Simultaneously close the left nostril as you lift your thumb from the right nostril.
- Exhale through the right nostril, 4 counts.
- Breath in through the right side, taking in a 4 count breath.
- Close the right nostril with the thumb and release the ring finger from the left nostril.
- Breathe out through the left nostril by, four counts.
- Repeat 5-10 times.
Physiologic Mechanisms: Studies demonstrated that synchronizing the two lobes of the brain during alternate nostril breathing increases cerebral hemisphere interaction. Research conducted with EEG monitoring reveals greater alpha-wave brain activity, associated with relaxed waking states of awareness. The latter method is also able to show observable effects in terms of heart rate variability and blood pressure regulation.
Applicability and Clinical Usefulness: This is a useful technique for anxiety presentations featuring the can’t stop/won’t stop nature of the thoughts, an inability to concentrate, and any sleep problems. The rhythmic counting and physical discipline involved provide cognitive anchoring, rather than a focus on anxiogenic stimuli.
Belly Breathing

Diaphragmatic breathing (also known as belly breathing) is the simplest therapeutic breathing exercise. This technique encourages good diaphragmatic support, while avoiding excitation of accessory muscles, which can be excessive in people suffering from chronic anxiety.
Clinical Application:
- Lie supine or sit in a chair with your back relaxed.
- Standing: Put one hand on your chest and another on your abdomen.
- Begin to breathe in through the nose and try to fill up your diaphragm
- The excursion of the abdominal hand should be greater than that of the chest hand.
- Now slowly exhale through the mouth and let the diaphragm recoil naturally.
- Continue for 5-10 minutes, using hand movement as biofeedback.
Physiological Explanation: This type of breathing has beneficial effects such as optimal ventilation-perfusion matching in the lungs, and activation of the vagus nerve by mechanoreceptors in the diaphragm. This vagal tone stimulation results in parasympathetic nervous system activation, resulting in diminished sympathetic outflow leading to decreased production of stress hormones. Septic diaphragm function The beneficial effect of the diaphragm on venous return and work of breathing.
Clinical Uses: This is the “kuti” (child) of all the other breathing exercises and is indicated in cases of paradoxical breathing. It is especially helpful for crisis type anxiety and can be done without anyone really noticing.
Box Breathing
Box breathing, sometimes known as square breathing or tactical breathing, is a breath exercise using equal periods of in- and exhale making a square-ended graph on the capnograph. This approach has been widely used in high-emotiom populations such as military or emergency responders.
Clinical Application:
- Hold the position with your feet planted on the ground and your back straight
- Full expiration to the FRC (functional residual capacity)
- Breathe in through your nose for a count of four
- Retain the breath (kumbhaka) four counts.
- Breathe out with mouth for 4 times
- Sustain the empty (post-expiration pause) for the duration of 4 counts
- Do 4-8 complete cycles of this exercise
Physiological Rationale: The matched equaltimeperiods of box breathing provide rhythmic activation of the baroreceptors and chemoreceptors, thus increasing heart rate variability (HRV) and baroreflex sensitivity. It imposes some much needed cognitive load, engaging your prefrontal cortex and reducing the activity in the amygdala — and it is in the amygdala where fear hormones are produced.
Box Breathing: Best use: Performance Anxiety, Acute stress or the need for immediate emotional support. The approach’s regimented nature renders it well-suited to those who are responsive to cognitive-behavioral treatments.
4-7-8 Breathing

The 4-7-8 breathing exercise, which was popularized by Dr. Andrew Weil and is based on an ancient yogic technique, promotes longer exhalation phases. This method is unique in that it focuses on the relaxation response with breath retention and long exhalation.
Clinical Application:
Place the tip of the tongue to touch the alveolar ridge behind the upper incisors
Exhale fully, powering all the air out of your lungs as you do. Breathe in through your nose for a count of four. That is one breath. Breathe in again, and repeat for a total of four breaths. Then, get your BLAST on with the countdown: whoosh out for eight counts, and then return to the count of four. REST of eight counts. Repeat for at least four cycles.
Close the mouth and inhale through the nostrils to the count of four.
- 7 seconds This is how long you should wait before exhaling.
- Breathe Out Completely through Your Mouth, making a “Whoosh” Sound, to a count of eight. Keep your lips shaped like an “O.”
- Start with 3-4 cycles, and slowly increase to as many as 8 cycles per session
Physiological Benefits: The prolonged exhale in 4-7-8 breathing greatly stimulates the parasympathetic nervous system. The breath-hold phase facilitates oxygen-CO2 exchange, while the extended exhalation activates the vagus nerve and induces release of GABA neurotransmitters; GABA is a potent anxiolytic.
Clinical Points: The application of this method has shown notable success among anxiety-insomnia patients and in cases of acute panic. The calming effects make it best to use in the equivalent of the evening or when you need to relax asap!
Lion’s Breath
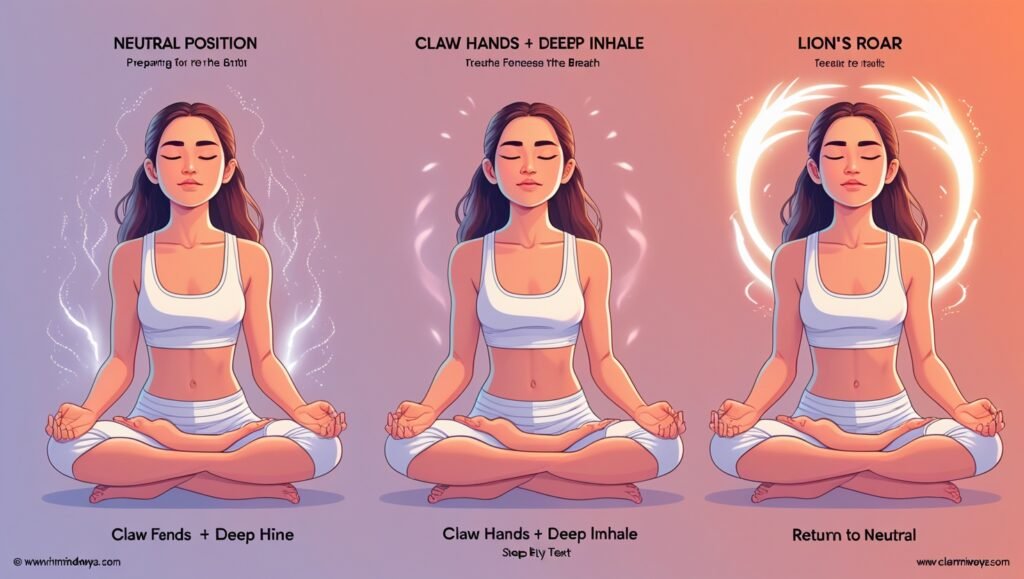
Lion’s Breath (Simhasana Pranayama) Lion’s breath is a controlled pranayama breathing exercise where you engage your facial muscles and voice. It’s a treatment that treats anxiety on both physiological and psychological levels, releasing physical tension and allowing you to express yourself emotionally.
Clinical Application:
- Sitting with hands on knees or thighs in comfortable poistion
- Stretch fingers like a claw and hook them.
- Breathe in deeply through the nose
- open the mouth wide, stick the tongue out toward chin and look up all at the same time.
- Blow forcefully out of your mouth and make a Ha or roaring sound
- Return to neutral position
- 3-7 more times with awareness of physical sensations.
Physiological Aspects: Lion’s breath requires you to work your face, neck, and throat muscles, helping you to relieve tightness in areas on your face that hold on to tension and stress. The expression itself allows for an emotional release and can activate vagal nerve pathways. It also encourages oxygen consumption and triggers the release of endorphins as the body is exerted.
Clinical Applications: Anxiety presentations with somatic tension, repressed emotions, or powerlessness can respond very well to this dynamic developmental intervention. It’s just that you can’t use it where vocalization would be out of place. (There’s ways to adapt for silent practice.)
Mindfulness Breathing
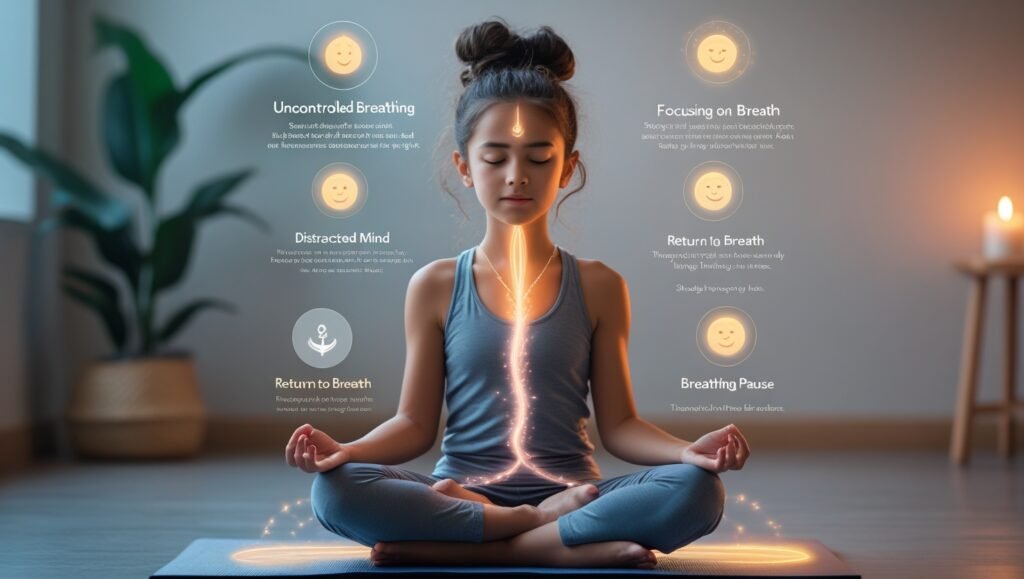
MB combines controlled breathing with present- moment awareness of the breath, thereby encompassing both cardiac and cognitive processing. It’s an approach informed by mindfulness-based stress reduction (MBSR) and is well supported by research.
Clinical Application:
- Sit comfortable with a straight spine
- Start out with regular uncontrolle breathing patterns
- Bring focus to the sensations of breath (nasal air flow, chest rising, or belly expanding)
- When the mind gets caught up in anxious thoughts, learn to notice without judging
- Softly bring attention back to the selected breath anchor
- Note how the pause from the in breath to the out breath feels natural
- Repeat for 5-20 minutes, depending on personal practice capabilities
Physiological mechanisms: MBTs have been shown to affect the structure and functioning of the brain. Neuroimaging evidence reveals a reduced amygdalar response and an enhanced activity of prefrontal cortex. Regular meditation strengthens default mode network control and rewires the emotional regulation circuitry.
Clinical Recommendations: This approach is best suited for people with generalised anxiety, who tend to ruminate, or who wish to build long-term resilience. It works particularly well when combined with other mindfulness-based treatments.
Pursed-Lip Breathing

Pursed-lip breathing is a clinical strategy to regulate expiratory flow by forcing lips to be partially closed. Developed initially for COPD patients, this has been shown to be effective in anxiety related breathing problems.
Clinical Application:
- Set yourself up into a comfortable lifting device in nice relaxed shoulder position.
- inhale slowly through the nose,” 2 counts, keeping mouth closed,
- p0008-5736 open Whistle Do a hole as small as you can by removing your pink lips so only your upper lip is more or less over the lower lip.
- Slowly exhale through pursed lips to a count of four counters.
- Keep it 1:2 inhalation to exhalation ratio
- Repeat for 5-10 breaths.
Physiologic Effects: Pursed-lip breathing generates positive expiratory pressure, which prevents airway collapse and enhances the efficiency of ventilation. Controlled exhalation precludes the entrapment of air and hyperventilation, and therefore also enhances the complete elimination of CO(2). This method also involves respiratory muscles to a greater extent as compared to uncontrolled breathing.
Clinical Applications Exposure to a fine stream of water is useful in most panic attacks, hyperventilation states and sense of breathlessness. It’s a good match for presentations of anxiety with lots of physical symptoms, too.
Resonance Breathing
Resonance or coherent breathing refers to breathing at a particular frequency around 5 breaths per minute (0.1 Hz). This approach maximizes heart rate variability and supports physiological coherence among the cardiovascular, respiratory and nervous systems.
Clinical Application:
- Sit or lie down in a comfortable position.
- Breathe in through your nose for 6 seconds
- Breathe out through the nose for 6 counts.
- Never stop the airflow as long as we are exhaling smooth and continuously without holding it.
- Keep this up for about 10-20 minutes
- Following a steady rhythm through an app or timing device
Mechanism of action: The synchronization between respiratory and heart rate patterns (in particular at the frequency of 0.1 Hz) determines a favorable balance between para-sympathetic and sympathetic systems control of the autonomic nervous modulation. At this frequency of 0.1 Hz, which is the natural frequency of baroreflex oscillations, maximal heart rate variability amplitude is achieved, which is associated with effective response to stress and better emotional regulation.
Clinical Applications: Resonance breathing is an excellent tool for Long Term Stress Management, general management of chronic anxiety disorders and building overall stress resilience. Training regularly shows an accumulation of effects and a possible enhancement of baseline autonomic function.
Simple Diaphragmatic Breathing Exercise
This clinical diaphragm breathing exercise is a systematic method to introduce participants to the human body’s natural breathing mechanics. It is both a treatment procedure and a diagnostic test for breathing pattern disorders.
Clinical Application:
- Lying supine with knees flexed and feet flat on the floor
- Place a hand on the chest and a hand on the abdomen
- Begin slow nasal breath, with attention to abdominal breath.
- Abdominal hand should move more than chest hand
- Draw in your stomach slightly as you slowly exhale from your mouth
- Practice this exercise for 5-10 minutes, 3-4 times each day and the habit should develop unconciously.
Physiological Mechanism: The right way of breathing through diaphragmatic breathing yields maximum tidal volume with minimal respiratory effort. It enhances ventilatory efficiency, decreases use of accessory muscles and leads to parasympathetic and vagal tone activation. This method also facilitates lymphatic drainage and venous return.
Clinical Rationale: This is the cornerstone exercise for those with dysfunctional breathing patterns and as a pre-cursor to more advanced exercise techniques. It’s especially true for people who suffer from chronic anxiety and have developed compensatory breathing patterns.
Chest Breathing vs. Abdominal Breathing
Chest breathing primarily utilizes the intercostal and accessory muscles of respiration rather than the diaphragm. This sign of pulsus paradoxus is relatively very uncommon and manifests as a chest rise and shoulder movement during inspiration.
Thoracic Breathing Qualities:
- Tachypnoea (often > 20 breaths per minute)
- Shallow tidal volumes
- You can also expect a lot of chest and shoulders.
- Minimal abdominal excursion
- Characters: Frequently associated with mouth breathin
- Can cause hyperventilation and respiratory alkalosis
- More breathing work and more job effort
Pathophysiological Effects: Durable thoracic respiration patterns may reinforce anxiety for several reasons. Hypocapnia (low CO2) can cause cerebral vasoconstriction resulting in hyperventilation, and anxiety symptoms. Furthermore, the activation of accessory muscles induces physical tension and provides the signals of stress for the central nervous system.
Diaphragmatic (Abdominal) Breathing
Diaphragmatic breathing is the ideal pattern of respiratory mechanics, which minimizes the use of the diaphragm as a muscle of respiration. This is described as abdominal movement that occurs on inspiration with minimal movement of the upper chest.
Diaphragmatic Breathing Characteristics:
- Reduced respiration frequency(around 8-12 breaths per minute)
- Deeper tidal volumes
- Prominent abdominal movement
- Minimal chest elevation
- Primarily nasal breathing
- Balanced blood gas tensions are preserved
- A reduced work of breathing
Physiological Benefits: Diaphragmatic breathing enhances gas exchange efficiency and cardiovascular advantages by enhancing the venous return. The rhythmic movement of the diaphragm also gives a kind internal massage to the organs of the abdomen, and by gently stimulating the vagus nerve it helps to facilitate parasympathetic tones.
Diaphragmatic Breathing Training: Switching from chest to belly breathing needs to be practiced with orderliness, and this task is often facilitated by a specialist. It is a program of neuromuscular re-education and the first experience for some — those who always breathe with their chest — can be quite uncomfortable.
How Can I Tell If I’m Breathing Properly?
Accurate assessment of breathing is key to ensuring effective treatment of anxiety. Not everyone is conscious of their breathing and many might not know they are breathing in a way that can exacerbate symptoms of anxiety.
Barometers Of Optimal Breathing :
- Diaphragmatic tone/abdominal expansion during inspiration
- Breathing 8-12 breaths per minute at rest
- Do effortless breathing with no audible sounds (this is the one you use in the exercises).
- Shoulder and neck position in respiration (1=neutral; 2=extended)
- Being able to rest comfortably between breaths
- Inclination to exhale with slightly longer phases in exhalation than inhalation
- You feel a calm, a centeredness when you focus on your breath.
Symptoms suggestive of dysfunctional breathing:
- Elevated chest and shoulder with inspiration visible
- Fast or erratic breathing
- Heavy sighing or sighs to get enough air.
- Jaw, neck or shoulder muscles feeling tight when breathing
- Feeling of shortness of breath or difficulty breathing
- Frequent yawning even after a full night’s sleep
- Symptoms of over-breathing (a light headed feeling/stinging sensation)
Clinical Sign: Two hands are used one on the chest and the other on the stomach. Right doing most of work. Determine which hand moves more during quiet breathing. Ideal breathing will demonstrate more movement through the abdomen and less through the chest. It is easy can be done throughout the day to build up the awareness of your breath.
Monitoring Breathing Patterns: Becoming mindful of your breathing patterns through the day is important in recognizing anxiety induced changes. Observe your inhalations and exhalations during various activities, with different amounts of stress, and in various emotional moods. That way, you can step in early with some relaxation techniques for breathing before the anxiety gets to be too much.
Professional assessment: The formal assessment by a respiratory therapist, a physiotherapist trained in breathing disorders or a health-care professional trained to eval uate breathing patterns may be of benefit to persons with chronic symptoms of breathing problems or of intense anxiety-related breathing symptoms.
Keep in Mind
Though breathing retraining is a nonspecific and benign technique for anxiety reduction, certain clinical issues must be taken into account in order to obtain maximum results and minimize negative repercussions.
Progressive Protocol of Breathing: Begin breathing training in short epochs (2 to 5 minutes) with progression as tolerance is developed. Quick advancement to longer sessions may lead to lightheaddedness, hyperventilation, or increased anxiety for persons who are sensitive. For each method, give yourself 1 to 2 weeks to adjust before moving on to more complicated exercises.
It’s About The Long Game, Not Just Training Sessions Research also shows that daily, shorter practices result in better outcomes than less frequent, longer ones. Develop a daily discipline of practice, at the same time each day if possible, to induce a conditioned relaxation response. Even extremely modest amounts of dedicated daily practice can create demonstrable changes in physiology.
Variability of individual responses: The efficacy of the breathing technique varies greatly among subjects, because of different patterns of breathing disorders, patterns of anxiety, physical limitations, and personal preference. Some of us gravitate to tally-ing methods; others to mindfulness techniques. Systematic testing of methods is suggested to determine the most effective interventions.
9Medical Considerations For those with respiratory diseases or conditions such as asthma, chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, heart disease, or any other medical conditions, it is advisable to consult health care professionals before starting with breathing training programs. Specific methods may need to be adjusted or could be inappropriate, depending on the neurologic condition.
Potential Side Effects: When used properly, breathwork tends to be very safe, but the following side effects are possible, particularly when you are beginning these practices:
- Slight feelings of dizziness or light headiness because of changes in the blood oxygen/carbon dioxide levels
- Temporary paresthesia (over-breathing results in a drop in blood carbon dioxide levels) in the hands and feet may occur.
- Emotional release or progressive anxiety as the autonomic balance tips
- Physical discomfort from unaccustomed breathing Insets and refernces?
Such effects usually disappear over time as the nervous system gets used to new ways of breathing. Any Symptoms which are frequent or severe should be evaluated by a healthcare professional.
Supplement Comprehensive Care: Use of profound breathing techniques should be supplemental and not a substitution for comprehensive types of treatment for anxiety. Pharmacological and non-pharmacological (i.e. cognitive-behavioral therapy, medical therapy, lifestyle changes and friendship) evidence-based treatments of anxiety must continue to be considered.
Clinical Cues For Professional Help: Professional mental health help is indicated when the following are experienced:
- Panic attacks resistant to breathing techniques
- High-anxiety – cannot work/ cannot function.
- Physical complaints leading to the consultation of a physician
- Never thoughts of self-harmque Suicidal thoughts / intent
- Labile deterioration of anxiety pattern with sustained practice.
Optimize your environment: Reduce distractions, ensure a comfortable temperature and use comfortable seating or lying position to practice breathing exercises. Some lone wolves need regular practice locations to reinforce conditioned relaxation responses.
5) Realistic expectations: This technique produces results with regular practice over weeks to months to reach maximum therapeutic effect. These adaptations may occur very quickly in some people, while others need extended periods of adaptation. Keep expectations in check and focus on improvement not cure right away.
Technology Integration: Smartphone apps and biofeedback devices can facilitate breathing exercise implementation through cues for timing, guidance for progress, and feedback on physiology. But these tools are meant to complement in the service of becoming our own experts in knowing what s going on within us via our breathing.
Interventions for Medical Emergencies: As discussed, breathing exercises are an effective technique for addressing symptoms of anxiety, not for medical emergencies. In cases of severe respiratory distress, chest pain or other acute medical symptoms, medical attention should be sought rather than interventions in breathing exercises.
Through the consistent use of this and other evidence-based breathing exercises, people can build practical competences, to help them control anxiety and, over time, become more and more resilient with respect to stress-related disorders. Success lies in regular use, choosing sensible techniques to apply, and supplementing with comprehensive anxiety treatment.